14 Feb 2025
By Stephanie Kleewein, Communications Manager, QuidelOrtho
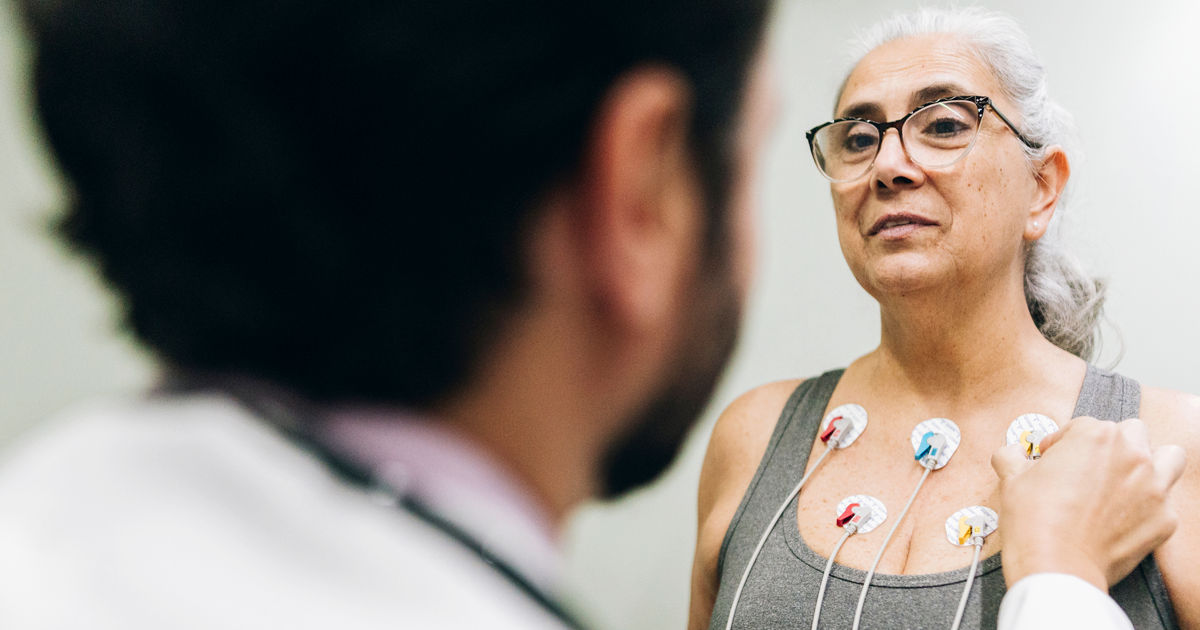
In an emergency room, decisions happen fast. A patient arrives with chest pain. Doctors, nurses, and staff move quickly, assessing symptoms, ordering tests, and preparing for the worst while hoping for the best. In cardiac emergencies, every second holds the power to save a life.
Advancements in point-of-care (POC) cardiac testing, combined with real-time patient monitoring, are changing how emergency departments (EDs) handle suspected heart conditions. These technologies are making diagnosis faster, improving outcomes, and helping emergency teams manage patient care with greater precision.
For years, emergency clinicians relied on traditional lab testing for critical cardiac biomarkers. It worked, but it took time, which cardiac patients do not often have. Today, POC testing delivers results in minutes. That speed allows doctors to move from suspicion to certainty much faster, helping them start treatment before a crisis escalates.
But speed alone isn’t the breakthrough. What makes POC testing so powerful is how it helps clinicians assess risk. It gives them the ability to sort patients quickly, ensuring those in immediate danger get the care they need while avoiding unnecessary hospitalizations for those who are stable. In a busy ED, where every second and every bed matters, that efficiency saves lives.
A fast result means little if it isn’t precise. Advances in POC testing have made huge strides in accuracy, reducing false negatives that could delay care and false positives that lead to unnecessary interventions. These tests work best as part of a broader approach, one that considers clinical judgment, patient history, and other diagnostic tools.
New multi-marker panels have also raised the bar. By measuring troponin, CK-MB, and myoglobin simultaneously, these panels provide a clearer picture of a patient’s cardiac status. Instead of relying on a single marker, clinicians get a more complete story that helps them distinguish between different cardiac conditions and determine the right course of action.
Through a process called apheresis, donors can also give specific components of blood such as platelets or plasma. Different from a whole blood donation where the blood is collected directly into a bag, with apheresis, blood is drawn from the donor into a machine that separates and collects the blood components using centrifugation. The remaining blood components are then returned to the donor from the machine.
Diagnosis goes beyond a single moment in time to understanding how a patient’s condition evolves. That’s why integrating POC testing with continuous patient monitoring is so important.
Real-time ECG readings and vital sign tracking complement biomarker testing, giving clinicians a more dynamic view of a patient’s heart. Subtle changes that might go unnoticed in a standard exam can be detected early, allowing emergency teams to adjust treatment, escalate care when needed, and, in some cases, intervene before a patient’s condition worsens.
While the impact of these tools can improve individual patient care, they are also reshaping how emergency departments function overall. Faster diagnosis means smoother patient flow. It reduces unnecessary admissions, helps EDs manage high volumes, and prevents overcrowding.
When low-risk patients can be safely discharged sooner, it frees up space for those who need critical care. It also leads to a better experience for patients, with less waiting, more certainty, and the confidence that they’re getting the right level of care at the right time.
The next wave of innovation is already taking shape. New biomarkers with even greater sensitivity are in development, making earlier detection possible and refining risk assessment. Advancements like these empower clinicians to detect cardiac events at their earliest stages before symptoms escalate into life-threatening emergencies.
Artificial intelligence and machine learning are transforming point-of-care diagnostics, analyzing vast amounts of patient data in real time, with the potential to recognize subtle patterns, flag high-risk cases, and support clinical decision-making with an unprecedented level of precision. By integrating AI with continuous monitoring, ED teams could anticipate changes in a patient’s condition faster and tailor interventions more effectively.
Innovation moves quickly, but its purpose remains constant—giving medical teams the ability to make better decisions under pressure. Faster, more accurate testing strengthens their ability to provide timely, targeted care. When seconds can make the difference between recovery and crisis, these breakthroughs bring more than efficiency. They bring the power to save lives.
Go to POC cardiac testing for more information.